Percutaneous Occlusion of the Auricle
Percutaneous occlusion of the left auricle is a procedure that consists of positioning special endovascular prostheses that occlude the left auricle.
Indice dell'articolo
Why is percutaneous occlusion of the auricle performed?
Atrial fibrillation is the most common and sustained arrhythmia, affecting 3-5% of the general population over the age of 65 and more than 13% of people over the age of 80. Stroke is the third leading cause of mortality, which in most cases is responsible for a profound psycho-physical disability. Atrial fibrillation is the cause of about 20% of all cerebral ischemic events, with an annual frequency that ranges from 2% to over 10% of cases. Most of the cerebral ischemic events associated with atrial fibrillation are due to thromboembolism starting from the left auricle.
The effectiveness of chronic anticoagulant therapy to prevent ischemic attacks in patients with atrial fibrillation has been well documented. For these considerations, current international guidelines recommend the long-term use of anticoagulant drugs to prevent acute cerebral ischemic events in all patients with atrial fibrillation without valve problems who are at risk of this complication. Unfortunately, despite these clear indications, chronic oral anticoagulant therapy cannot be used in all patients for several reasons.
Considering the problems related to chronic therapy with oral anticoagulants in patients with non-valvular atrial fibrillation, in recent years effective and safe alternative therapeutic strategies have been researched and evaluated. A therapeutic strategy that is essentially based on the prevention of thrombo-embolic events, called occlusion of the left auricle, is considered, and carried out transcutaneously via a catheter. The prevention of thrombi from the left auricle causes the elimination or significant reduction of the risk of stroke.
What is percutaneous occlusion of the left auricle?
Percutaneous occlusion of the left auricle is a procedure that consists of positioning special endovascular prostheses that occlude the left auricle. The left auricle is a bag-shaped structure located in the antero-superior portion of the left atrium. Its anatomical structure particularly favors the formation of thrombi (blood clots) during atrial fibrillation.

In fact, numerous studies show that over 90% of cases of left atrial thrombosis during atrial fibrillation form in the left auricle.
Auricular thrombosis is a known and particularly dangerous complication of atrial fibrillation and, for this reason, requires patients with atrial fibrillation to be treated with anticoagulant drugs, that is, with medicines that reduce the natural ability of the blood to form clots.
However, there are different conditions that make this anticoagulant therapy contraindicated, impractical or not completely effective.
In which patients is percutaneous occlusion of the auricle recommended?
Patients with high bleeding risk, such as patients with cerebral vascular malformations, blood diseases, malignancies, severe renal and hepatic insufficiency, or other conditions that promote bleeding, have such a high risk of bleeding during anticoagulation therapy that they cannot receive such treatment in sufficient safety.
There are also conditions in which patients are unable to take anticoagulant therapy with the necessary therapeutic continuity or who experience episodes of auricular thrombosis even in the presence of anticoagulant therapy at the highest therapeutic levels.
In these patients, percutaneous occlusion of the left auricle is the only effective therapeutic alternative for the prevention of atrial thrombosis.
At present, the indications for percutaneous occlusion of the auricle are as follows:
• Evidence of recurrent atrial thrombosis in optimal anticoagulant therapy. |
How is percutaneous occlusion of the auricle performed?
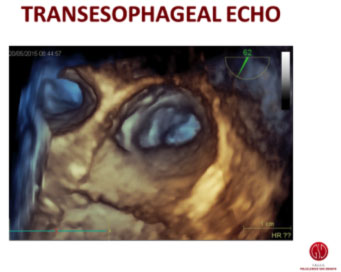
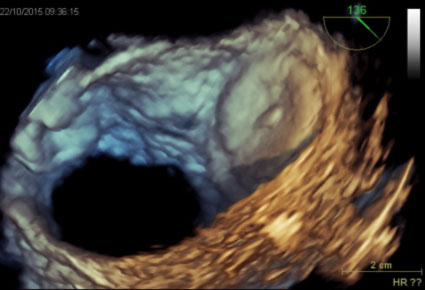
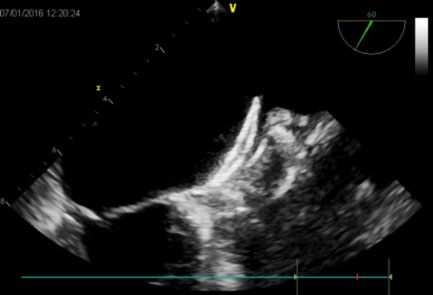
The occlusion procedure of the left auricle is performed under general anesthesia and under transesophageal fluoroscopic and echocardiographic guidance.
The patient is prepared as for a standard transcatheter procedure with effective anticoagulation, which must be maintained during and after the procedure.
Using a transseptal cardiac catheterization, a guide catheter is positioned in the left auricle and images of the ear cavity are acquired in order to allow an accurate measurement of its diameters. The size of the prosthesis is decided on the basis of the diameters measured angiographically and with the transesophageal echocardiogram.
Different types of endovascular occluders are currently available, consisting of a cage of superelastic metal material (nitinol) capable of anchoring to the internal surface of the auricle and completely occluding it. By excluding the auricular cavity from the circulation, these prostheses prevent thrombi from forming inside it, thus definitively eliminating the thrombogenic potential of the auricular.

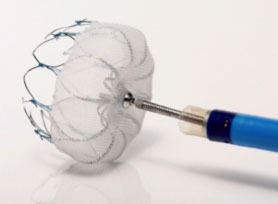
Once the most suitable type and size of prosthesis has been chosen, it is inserted and released inside the auricle through the guide catheter, assessing its correct and stable positioning by means of traction maneuvers performed under ultrasound and radioscopic control. Once a complete occlusion of the auricle has been obtained at the level of its host, and after confirming the stability of the prosthesis, the prosthesis itself is released.
Is antithrombotic therapy required before percutaneous occlusion of the auricle?
Before the procedure, aspirin (81–325 mg / day) and clopidogrel (75 mg / day) is recommended up to 48 hours before the procedure. Antibiotics must be administered 1 hour before surgery. Intravenous heparin boluses will be administered after the transseptal puncture. After the closure of the auricle, patients will remain on chronic aspirin therapy (81–325 mg).
What are the contraindications to percutaneous occlusion of the auricle?
There are few contraindications to its application if the presence of an intracardiac thrombus, an endocardial infection in the activity phase or in the presence of an infection (bacteremia), or the presence of other intracardiac devices (automatic implantable defibrillators) and / or intravascular are excluded, which could potentially interfere with its positioning.
How is the device checked after the procedure?
One day after the procedure, a chest X-ray and a trantoracic echocardiographic examination are performed to rule out an asymptomatic pericardial effusion or a poor positioning of the device. In the absence of contraindications, the patient can be discharged in 1-2 days. An echocardiographic examination is scheduled after 4 weeks, 3 months, and every 6 months.
After percutaneous occlusion of the auricle, must the patient continue anticoagulant therapy?
After the auricle occlusion procedure, the patient will no longer need anticoagulant therapy, but will have to take a double antiplatelet therapy for 3 months, and then remain in treatment with low-dose aspirin.
What are the risks of percutaneous occlusion of the auricle?
Like all invasive procedures, percutaneous occlusion of the auricle has a risk, albeit minimal, of complications. The most frequent complications are local ones that include a small hematoma at the site of introduction of the catheters, while, much rarer are the lesions affecting the blood vessels or nerves that run in the vicinity of the vessels. Injuries to the vessels in the vicinity of the heart or in the heart itself occur with an extremely low frequency. More frequently, the complications are transient (mild self-absorption hematoma, transient chest pain) or correctable.
In rare cases, more serious complications may occur, requiring circulation support (through ECMO) and cardiopulmonary resuscitation maneuvers. The patient may be exposed to risks of major complications starting from those related to the transactal puncture, and which include cardiac tamponade and / or gas embolism. In rare cases, it is possible that a perforation of the heart with a collection of blood in the pericardium (hemopericardium) may occur, which requires a pericardiocentesis (drainage of the pericardium) or, even more rarely, the need for surgery.
In centers experienced in this type of transcutaneous approach, the procedure can be performed quickly and optimally, and from the data reported recently, with an extremely low frequency of complications, usually less than 1%.
In any case, in our center, during percutaneous occlusion of the auricle, in addition to electrophysiologists, there are always also specialist anesthesiologists, and the procedure is generally carried out in a hybrid room (i.e. a room specifically equipped in case it is necessary to intervene with ECMO or with a cardiac surgery procedure).
In summary, the risk associated with percutaneous occlusion of the auricle is low, and the advantage derived from its use for the patient with the correct indications is considerable. Transcutaneous occlusion of the left auricle therefore represents a valid alternative to long-term oral anticoagulant therapy for the prevention of cerebral ischemic attacks in patients with non-valvular atrial fibrillation.
