Familial Dilated Cardiomyopathy
Indice dell'articolo
What is Familial Dilated Cardiomyopathy (DCM)?
Familial dilated cardiomyopathy (DCM) is a heart muscle disease characterized by ventricular dilation and reduced systolic function. Patients have heart failure, arrhythmias, and an increased risk of sudden cardiac death (SCD). The prevalence of DCM is 1/2,500, with an incidence of 7/100,000 cases per year (although this incidence is probably underestimated). In many cases, the disease is inherited and is therefore referred to as familial DCM (FDCM). FDCM corresponds to about 20-48% of DCM cases, usually with autosomal dominant transmission. DCM is caused by mutations in the genes that code for cytoskeletal and sarcomeric proteins of cardiac muscle cells. One of the most important genes is LMNA, also responsible for other forms of arrhythmias (Bengala et al, 2019).
What is the clinical presentation of Dilated Cardiomyopathy (DCM)?
DCM is a progressive and usually irreversible pathology of the myocardial muscle, which leads to systolic and dilated dysfunction of the left ventricle. Clinically, it can occur with heart failure, supraventricular and ventricular arrhythmias, thromboembolism, and sudden death. DCM diagnosis requires the exclusion of a secondary cause, particularly ischemia. The mortality rate of the disease is high (12-20%), even in the population receiving optimal medical treatment, mainly due to heart failure and ventricular arrhythmias that result in SCD. The symptoms of DCM are those of heart failure (weakness, easy fatigue, labored breathing during sometimes even moderate effort, persistent dry cough, swelling of the abdomen and lower limbs, sudden weight gain caused by water retention, loss of appetite) and cardiac arrhythmias (palpitations, dizziness or fainting).
What are the diagnostic tests for Dilated Cardiomyopathy (DCM)?
The following tests are recommended for symptoms resulting in the suspicion of DCM:
Blood chemistry tests: A risk marker is the dosage of brain natriuretic peptide (BNP), which is elevated in the presence of heart failure. Changes in the liver and kidney function indices may also be present, an expression of the suffering of these organs due to heart failure. In severe cases, there is hyposodyemia, hypokalaemia and anemia.
Chest X-ray: provides information on the size of the heart and the presence and degree of lung congestion.
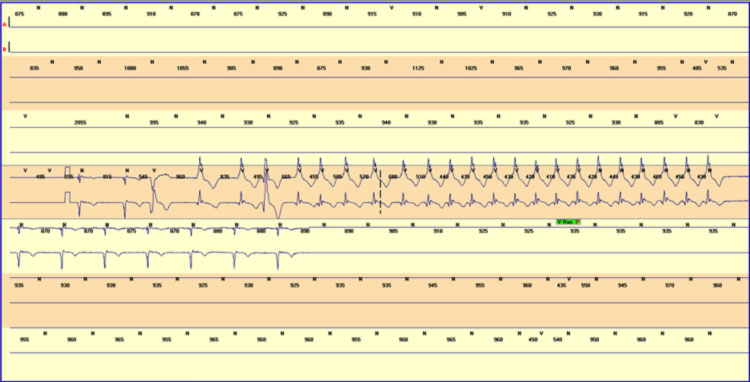
Basal ECG and dynamic Holter ECG: The electrocardiographic markers of arrhythmic risk may include the presence of fragmented QRS and the presence of micro-alternation of the T wave, even if these parameters have not yet been assessed prospectively. Other ECG markers are the recognition of supraventricular or ventricular arrhythmias, in particular unsustained ventricular tachycardias during Holter recording, usually detected by prolonged Holter monitoring.
Echocardiogram: It is the fundamental examination for the diagnosis and follow-up of DCM, as it allows to evaluate the size and thickness of the walls of the cardiac chambers, the contractile function (measured with a parameter called “left ventricular ejection fraction (LVEF)) and valve function, and to estimate lung pressure. The presence of a LVEF < 35% is considered a negative prognostic index, associated with a high risk of SCD.
Stress test with oxygen consumption: The exam consists of recording an electrocardiogram while the patient performs physical exercise, generally walking on a treadmill or pedaling on an exercise bike; a mouthpiece for the measurement of exhaled gas is also applied. The test allows to evaluate the subject’s resistance to exercise, the presence of desaturation during exercise, the appearance of signs of ischemia and arrhythmias under stress.
Coronary angiography: these tests serve to exclude the presence of significant coronary artery disease or the presence of congenital anomalies of the coronary artery.
Cardiac magnetic resonance imaging (cMRI) with contrast medium: The examination allows a better assessment of the right ventricle compared to the echocardiogram, and also assesses the structure of the myocardium, thus allowing to identify the presence of inflammatory processes and areas of intramyocardial fibrosis (scars). Myocardial fibrosis is a significant feature of dilated cardiomyopathy, and provides the substrate for ventricular arrhythmias, as it predisposes to the formation of re-entry circuits. Fibrosis is generally localized in the myocardial wall (mid-wall fibrosis).
Cardiac catheterization: is an invasive method that is based on the introduction of a catheter through a venous vessel up to the right cavities of the heart, which allows to acquire important information on the flow and oxygenation of the blood and on the pressure inside the right heart chambers and on the lung pressure. This is an examination reserved for the most serious forms in which it is necessary to verify the degree of increase in the ventricular filling pressures and the reduction in cardiac output (i.e. the amount of blood pumped by the heart) and pulmonary hypertension.
Endomyocardial biopsy: is performed during the execution of cardiac catheterization by using a tool called a biotome. Typically biopsies are performed on the right side of the interventricular septum. It is indicated in patients with recently found dilated cardiomyopathy and “fulminant” heart failure to identify the presence of myocarditis and, if necessary, identify the type of cells that support the inflammatory process, because this has an important prognostic value.
What are the treatments for Dilated Cardiomyopathy (DCM)?
The treatment of DCM is essentially therapy to treat and prevent heart failure and arrhythmias, to improve symptoms, and increase survival. Currently, heart failure therapy includes general measures (controlled intake of salt and liquids, treatment of hypertension, limitation of alcohol intake, control of body weight, moderate exercise), followed by the use of drugs and heart devices:
Drugs: ACE inhibitors, sartans, beta-blockers, anti-aldosterones, diuretics, digoxin.
Cardiac devices: pacemaker (PM), resynchronizers (CRT), intravenous cardiac defibrillators (ICD).
In cases refractory to medical and electrical treatments, the implantation of left ventricular assist devices (LVAD) and heart transplantation are indicated.
What are the current recommendations for the prevention of sudden death in dilated cardiomyopathy?
The current guidelines of the European Cardiology Society (ESC 2015) recommend the use of an implantable defibrillator (ICD) in primary prevention in patients with DCM in the New York Heart Association (NYHA) II and III class, and with a left ventricular ejection fraction (LVEF) less than or equal to 35%. LVEF is an important predictor of malignant ventricular arrhythmias in patients with DCM. The absolute risk of SCD increases with the worsening of LVEF. Even some recent trials (for example the DANISH study) have not shown a significant reduction in mortality in patients with ICD implantation in primary prevention, in comparison with only optimal medical therapy (OMT). In any case, current guidelines recommend ICD implantation after at least 3 months of optimal drug therapy with ACE inhibitors, beta-blockers and diuretics, since, in some patients, a more or less partial recovery of LVEF can be observed after at least 3 months of OMT.
What is the role of genetics in dilated cardiomyopathy?
DCM is associated with mutations in the genes that code for cytoskeletal and sarcomeric proteins of cardiac muscle cells. One of the most important genes is LMNA, which codes for Lamina A and C. Patients in whom the genetic mutation is identified appear to be at greater risk of SCD with a mortality of 40% at 5 years. Therefore, the earliest implantation of an ICD is recommended in patients with a genetic mutation of the LMNA gene.
In the case of familial dilated cardiomyopathy, the search for genetic mutations associated with the development of DCM is recommended. If a genetic mutation associated with the development of DCM is identified, the study of family members is naturally recommended, to identify other possible affected subjects within the family: those in whom the search for the mutation will be negative can be reassured that they will not develop the pathology, while the healthy carriers of a possible mutation must be followed over time (in particular with echocardiogram and ECG monitoring), to identify the possible clinical appearance of the disease.
To consult Orphanet
https://www.orpha.net/consor/cgi-bin/OC_Exp.php?Lng=IT&Expert=154
For bibliographical references:
If you want to know more > Cardiogenetics
