Unexpected Death
Unexpected Death is natural death in subjects with or without known pre-existing heart disease, but in which the timing and the manner of death are unpredictable.
Indice dell'articolo
What are cardiac arrest and sudden cardiac death?
Sudden cardiac death (SCD) is an unexpected death of cardiac origin. The definition of SCD, according to Myerburg (1980) is a “natural death, preceded by a sudden loss of consciousness, which occurs within 1 hour from the onset of symptoms, in subjects with or without known pre-existing heart disease, but in which the timing and the manner of death are unpredictable.”
Normally, “sudden cardiac death” and “cardiac arrest” are considered as synonymous, even though from a physiopathological point of view, sudden cardiac death is a consequence of cardiac arrest, i.e. from the cessation of the heart pump function, and therefore from the interruption of blood circulation to the whole body.
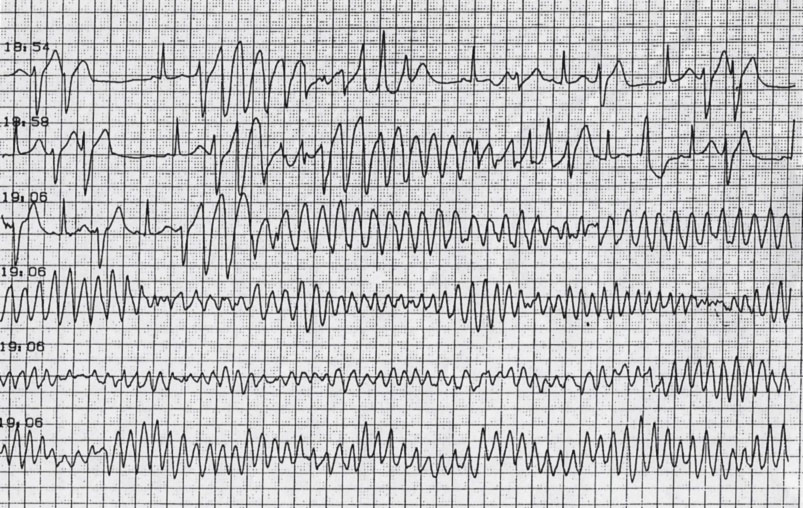
In about 70-80% of cases, cardiac arrest is caused by a tachyarrhythmia, i.e. a rapid and disorganized ventricular arrhythmia, called ventricular fibrillation. In other cases, cardiac arrest may be due to a bradyarrhythmia, or a slowing of cardiac function.
Cardiac arrest is rapidly followed by circulatory arrest and a drop in blood pressure with consequent loss of consciousness, generally within 10-15 seconds. After a few moments, the non-perfusion of the respiratory centers leads to respiratory arrest, and within four minutes after the cardiac arrest, the brain cells begin to die and irreversible neuronal damage occurs due to the lack of oxygenated blood supply.
Sudden death can be reversible through timely and adequate resuscitation maneuvers, but leads inevitably to death if not properly and rapidly treated. Unfortunately, however, despite timely therapy, the death of the individual, or brain damage, cannot always be avoided.
What is the incidence of sudden cardiac death in the general population?
The incidence of sudden death is about 1/1000 individuals per year and increases to about 8/1000 subjects a year with a history of heart disease. Sudden cardiac death is responsible for about 50,000 deaths a year in Italy. Sudden cardiac death represents over 50% of all cardiovascular disease deaths. About 80% of sudden cardiac deaths are caused by ischemic heart disease, mainly in the higher age groups. Conversely, in the younger age groups, the majority of arrhythmic cardiomyopathies, channelopathies, or congenital heart disease is undiagnosed.
Sudden death occurs mainly in males (about 60%) in all age groups. In particular, it is the main cause of death in males aged between 20 and 60 years. Sudden cardiac death can also affect children, particularly within the first 6-12 months of age, and it is often referred to as Sudden Infant Death Syndrome (SIDS).
What is the incidence of sudden cardiac death in athletes?
The first case of sudden death during sports activity was that of Filippide, who died suddenly immediately after announcing the victory of the Marathon to the Athenians.
Sudden cardiac death is a not infrequent event for athletes, both professionals and amateurs alike. The incidence of sudden death among athletes is similar to that of the general population. However, it is particularly shocking because it usually occurs in young individuals (under 35 years of age) who are apparently healthy, especially considering the level of physical activity that they perform, and considering the physical exams that they must undergo in Italy.
Cardiomyopathies most frequently associated with sudden death during exercise are arrhythmogenic right ventricular cardiomyopathy, and catecholaminergic polymorphic ventricular tachycardia (CVPT).
What are the causes of cardiac arrest and sudden death?
The underlying causes of cardiac arrest and sudden cardiac death can be multifold. The most frequent cause is ischemic heart disease (caused by an obstruction of the coronary arteries). However, especially in young people, additional causes are arrhythmic cardiomyopathies, channelopathies, or undiagnosed congenital heart disease.
Non-ischemic cardiopathies that are mainly associated with sudden cardiac death include:
- Hypertrophic cardiomyopathy, characterized by ventricular hypertrophy, in particular, of the left ventricle, generally with a family history and represents the primary cause of death in athletes under 35 years of age.
- Dilated cardiomyopathy, characterized by progressive dilatation of the cardiac chambers, which is associated with a thinning of the wall with consequent impairment of the functionality of the heart. Often this is also found in the family.
- Arrhythmogenic right ventricular dysplasia, characterized by fibro-adipose substitution of the ventricular myocardium, especially in the right ventricle, but may also involve the left one. Generally, it runs in the family and is caused by mutations located in specific genes and transmitted in an autosomal dominant manner.
- Noncompaction cardiomyopathy, with abnormal trabeculae in the walls of the left ventricle.
- Arrhythmogenic channelopathies, in particular Brugada syndrome (BrS), long QT syndrome (LQTS) and catecholaminergic polymorphic ventricular tachycardia (CPVT): these are cardiac pathologies in which the heart is morphologically normal, but there is the presence of anomalies and defects at the level of cardiac ion channels capable of favoring the onset of malignant ventricular arrhythmias and, consequently, of sudden cardiac death.
- Wolff-Parkinson-White syndrome, which includes the presence of atrio-ventricular conduction pathway anomalies.
- Congenital heart diseases, present at birth, for example, aortic stenosis and Tetralogy of Fallot.
- Congenital coronary artery disorders, also known as coronary artery disease (for example, narrowing or obstruction of the coronary arteries which, in turn, can lead to cardiac ischemia or myocardial infarction and, finally, to sudden cardiac death).
- Anomalies and pathologies of heart valves (aortic stenosis or bicuspid aortic valve, mitral prolapse, pulmonary artery stenosis).
What are the risk factors for sudden death?
The most important aspect of preventing sudden death is identifying those at risk early. The known risk factors for sudden death are as follows:
- Family history of sudden cardiac death.
- Low ventricular ejection fraction (i.e. the measure of heart function, which is measured non-invasively through the echocardiogram).
- History of ischemic heart disease and myocardial infarction.
- Cardiomyopathies (hypertrophic, dilated, non-compact myocardium, arrhythmogenic dysplasia).
- History of syncopes (fainting, loss of consciousness) due to unknown causes.
- History of supraventricular cardiac arrhythmias (including atrial fibrillation) and ventricular extrasystoles or unsupported ventricular tachycardias.
- Electrocardiographic abnormalities suggestive of channelopathies (Long QT syndrome, Brugada syndrome, Short QT syndrome, early repolarization).
- Atrio-ventricular or intraventricular conduction blocks.
Other factors that could increase the risk of sudden cardiac death are:
- Old age
- Smoking
- Diabetes
- Stress or strenuous exercise
- Dyslipidemia
- Alcohol abuse
- Use of drugs (in particular cocaine, amphetamines and other drugs)
- Use of certain types of drugs, known to have a potential pro-arrhythmic effect (in particular some antiarrhythmic drugs, antidepressants, antihistamines, antibiotics)
- Nutritional imbalances (anorexia, bulimia)
- Electrolyte imbalances (i.e. low blood levels of potassium or magnesium)
What are the signs of Sudden Cardiac Death?
In most cases, sudden cardiac death occurs, as its name suggests, in a sudden and unexpected manner and the patient loses consciousness and falls to the ground, appearing already lifeless.
In some cases, before reaching the loss of consciousness, patients may experience “warning signs” that indicate imminent cardiac arrest, such as:
- Localized pain in the center of the chest, similar to that of a stomach ache, which radiates to the arms, back, throat and even the jaw;
- Palpitation, that is, feeling of irregular heartbeat
- Cold sweats;
- Breathing difficulties, dyspnea and cough;
- Weakness, agitation;
- Nausea and vomit.
Unfortunately, however, these signs do not always manifest themselves, making it difficult, if not impossible, to recognize the imminent arrival of sudden cardiac death, which only becomes apparent with the onset of unconsciousness (called syncope).
What should be done in the event of cardiac arrest and sudden death?
In the case of cardiac arrest, when the blood flow and respiration stop, cardiopulmonary resuscitation is the emergency procedure that can maintain circulation and breathing until help arrives, and thus make the difference between life and death for the person in cardiac arrest.
| Therefore, if you are witnessing a cardiac arrest, it is always better to try cardiopulmonary resuscitation, even if you fear that your knowledge is insufficient, because doing something and doing nothing could be the difference between life and death or permanent brain damage to the affected person. |
In case you are witnessing a cardiac arrest, first you need to immediately call the emergency number (in Italy 118, but in some Italian regions 112). When you call, the attendant will probably ask you if you are able to practice cardiopulmonary resuscitation (CPR) with cardiac massage. If you don’t know how to do it, you will be instructed on the phone. The witnesses of the arrest should immediately begin the cardiac massage and continue until the ambulance arrives.
The cardiac massage consists of a rhythmic compression of the thorax, essential to guarantee the mechanical (pump) function of the heart that had ceased following the cardiac arrest. These mechanical compressions must continue until the ambulance arrives and the respondents are ready to apply the use of a defibrillator (give a shock).
| The rescuer’s hands should be placed “in the center of the chest”, on the sternum, about a palm’s length away from where the lowest ribs meet, resting the palm of one hand on the other hand. To ensure a useful cardiac massage, it is important to compress the chest to lower it by about 5-6 centimeters (in the adult person) and allow it to completely re-expand after each compression, while maintaining an adequate speed (about 100 – 120 compressions / minute). It is essential to never stop the cardiac massage, except for the time necessary to perform the ventilations or when indicated by the defibrillator’s voice commands. |
| The correct technique for performing cardiac massage is taught in Basic Life Support and Defibrillation (BLSD) courses, which are strongly recommended to the entire population. |
As soon as possible, external cardiac defibrillation should be attempted.
What is external cardiac defibrillation?
In the event of cardiac arrest, “early defibrillation” is essential, i.e. the delivery of an electric shock to the myocardium that interrupts ventricular tachycardia or ventricular fibrillation. This operation must be carried out within a few minutes of cardiac arrest so that it is effective, since delaying the operation decreases the possibility of survival, due to irreversible brain damage due to lack of oxygen.
The technique of administering this shock is called “defibrillation” and consists of the therapeutic use of electric current that is delivered in high quantities for a very short period of time. The purpose of defibrillation is to temporarily abolish all electrical activity of the heart through complete depolarization of the myocardium, allowing the natural pacemaker of the heart to resume its normal rhythmic activity.
The delivery of this electrical discharge occurs through the use of cardiac defibrillators: some models are implantable inside the chest (internal defibrillators) while others must be connected externally to the victim’s chest (external defibrillators).
External defibrillators are divided into:
- manual (or “conventional”), usable only and exclusively by medical personnel;
- automatic (AED), which can also be used by non-medical personnel.
| The automatic defibrillator (AED) requires only that the operator apply the pads to the patient, activate the instrument, and follow the verbal instructions that will be given by the device. In the event that a shockable rhythm is present, the instrument will recognize this. However, a person must continue to assist the patient, as directed by the AED. |
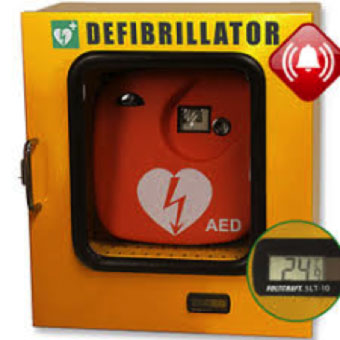
AEDs are currently increasingly available in public places (airports, railway stations, supermarkets, schools, hospitals, sports facilities, etc.) and are indicated by a special sign.

How to prevent sudden cardiac death?
The prevention of sudden death is possible in some cases. The most important aspect of preventing sudden death is identifying those at risk early.
The most important parameter is the ejection fraction. Other important parameters are the family history of sudden death, the personal history of heart disease, syncope and cardiac arrhythmias and the presence of specific electrocardiographic abnormalities (long QT, Brugada pattern, early repolarization).
If the patient is considered to be at risk of sudden death, non-invasive tests (Holter, exercise test), cardiogenetic tests and provocative invasive tests (pharmacological and electrophysiological) are available to specify (stratify) the level of risk of sudden death.
If the risk is considered high, you can intervene by implanting an implantable cardiac defibrillator (ICD) before a cardiac arrest has occurred, which, if necessary, intervenes with electric shocks that can restore the normal function of the heart.
In the case of patients surviving cardiac arrest, action is taken by implanting an implantable cardiac defibrillator (ICD).
In some situations, in which there is a history of recurrent ventricular arrhythmias, or in the case of Brugada syndrome, it is possible to intervene with radiofrequency transcatheter ablation of the arrhythmic substrate, significantly reducing the probability of the onset of fatal ventricular arrhythmias.
