Cardiac Magnetic Resonance
What does Cardiac Nuclear Magnetic Resonance consist of?
Cardiac nuclear magnetic resonance imaging (MRI) is a diagnostic test based on the application of a high intensity magnetic field to the chest, with the aim of visualizing cardiac structures and tissues. Compared to other imaging methods, it has several advantages: low invasiveness, absence of ionizing radiation, and images in three dimensions.
Different conditions, ranging from ischemic heart disease to cardiomyopathies, congenital heart disease, or valve abnormalities, share the possibility of triggering complex ventricular arrhythmias. To date, the most effective tool for the prevention of sudden arrhythmic death is the cardiac defibrillator (ICD) implant. Although the decision to implant a defibrillator for primary or secondary prevention of sudden arrhythmic death is fundamentally based on the definition of severe dysfunction of the left ventricular ejection fraction (LVFE ≤35%), this criterion alone has not proven to be specific or sensitive enough.
In fact, only a fifth of all patients who experience sudden death have an LVEF of ≤35%, and appropriate therapy by the ICD occurs in less than a third of patients undergoing implantation defibrillators due to evidence of LVEF of ≤35%. (1,2). On the other hand, lethal arrhythmic events often occur in patients with cardiomyopathies even if they have a preserved left ventricular function (LVEF ≥50%).
In this context, cardiac nuclear magnetic resonance imaging (MRI) is an extremely useful diagnostic tool by quantifying in a detailed way the volume of the cardiac chambers, the mass and the global and segmental function of the left and right ventricle, and analyzing the histology and cardiac morphology.
In which arrhythmogenic cardiopathies is Cardiac Nuclear Magnetic Resonance indicated?
The execution of a cardiac nuclear magnetic resonance exam plays a role of fundamental importance, especially in the study of arrhythmogenic substrates of the following pathologies associated with the risk of sudden death:
- Ischemic heart disease: It is the main cause of sudden death, above all due to the arrhythmogenicity of the post-infarct scar visible through the late gadolinium enhancement (LGE) technique. Several studies have correlated the presence and extent of LGE to the risk of malignant ventricular arrhythmia, sudden death and the occurrence of appropriate shock by the ICD (3).
- Primary Dilated Cardiomyopathy: Primary dilated heart disease is characterized by biventricular dilation not caused by ischemic conditions or by volume or pressure overload. Also in this case, the presence of fibrosis, detectable by LGE, was associated with the risk of malignant ventricular arrhythmia and sudden death. Furthermore, a reduced overall longitudinal strain has been independently associated in various studies with a composite endpoint comprising ventricular arrhythmias and sudden death (4).
- Hypertrophic cardiomyopathy: Hypertrophic cardiomyopathy is a genetic pathological condition characterized by extreme myocardial hypertrophy. The study with MRI enables the evaluation of the extension of the hypertrophic segments (global, septal, apical or middle ventricular hypertrophy), to evaluate the presence of elements associated with arrhythmogenic risk, such as left ventricular thickening> 30 mm, apical aneurysmal dilation, left ventricular ejection obstruction, the presence and extent of ischemia / fibrosis. All these elements have proven to be strong predictors of sudden death in patients with this condition (5, Figure 1).
- Arrhythmogenic Right Ventricular Dysplasia (ARVD): ARVD is a genetic pathology of the heart muscle characterized by a fibro-fat substitution of the right ventricular myocardium, but which can also affect the left ventricle in a variable percentage. According to the European Society of Cardiology, the diagnosis is based on the presence of major and minor diagnostic criteria, which include structural, histological, electrocardiographic and clinical elements, such as the family history of sudden death. In this context, cardiac magnetic resonance imaging plays a fundamental role in defining the size, global function, segmental kinetics of the right ventricle and histological characterization. In particular, the demonstration of fibro-fat substitution can guide the decision to implant an ICD (6, Figure 2).
- Sarcoidosis: Sarcoidosis is a granulomatous systemic disease involving the heart in 2-5% of cases. The presence of granulomas and possibly areas of focal fibrosis is associated in various studies with the risk of sudden death (7).
- Viral myocarditis: The most common cause of viral myocarditis in humans is Herpesvirus 6 (HHV6) and Parvovirus B19 infection. Sudden cardiac death occurs from 2 to 8.6% of cases and is associated with the presence of areas of LGE and the degree of acute global systolic dysfunction (8).
- Cardiomyopathy from iron accumulation: In hemochromatosis, the iron deposit of the myocardium is associated with the risk of ventricular arrhythmias. In this case, the T2 * relaxometry value correlates with the risk of malignant ventricular arrhythmia. In patients with T2 * <20 msec the relative risk of malignant ventricular arrhythmia is 4.60 times greater than in those with T2 *> 20 msec (9).
- Mitral valve prolapse: Mitral valve prolapse is a myxomatous degenerative valve heart disease affecting the valve system as a whole (ring, flaps, tendon cords) and which can be associated with mechanical stress of the papillary muscles and the lower wall of the left ventricle. The presence of LGE at the apex of the papillary muscle at the chordal insertion is associated with the presence of complex ventricular arrhythmias in 63% of patients suffering from mitral valve prolapse and a consequent increased risk of sudden death (10).
- Congenital heart disease: Congenital heart disease is an important cause of sudden death in the population under 30 years old, and especially in children. In this context, cardiac MRI enables the acquisition of important morphological and functional information, with the advantage of not administering ionizing radiation. For example, the presence of severe left, right ventricular dysfunction or the right outflow tract and the presence of LGE areas has proven to be able to predict in several studies the occurrence of adverse cardiovascular events in patients undergoing surgical correction of Tetralogy Fallot (11).
Are particular precautions required to perform Cardiac Nuclear Magnetic Resonance?
In general, there are no special preparations for undergoing cardiac magnetic resonance imaging. In rare cases, preventive treatments may be carried out to avoid allergic reactions in some people who must undergo the examination with contrast medium (Gadolinium). In case of particular allergies, the patient must inform our center in advance.
Which patients cannot undergo Cardiac Nuclear Magnetic Resonance?
Patients with pacemakers or defibrillators or cardiac resynchronizers not declared compatible, and carriers of implantable devices with magnetic activation – such as electrodes and neurostimulators – and wearers of prostheses that cannot be ascertained to be compatible with magnetic fields cannot undergo cardiac MRI. Patients with MRI compatible cardiac devices (MRI Conditional) must report the presence of the device at the time of booking, in order to schedule the examination in specific conditions.
See information for performing MRI in carriers of implantable cardiac devices
Information for cardiac device users by the manufacturing companies
In general, cardiac MRI is not recommended in the first trimester of pregnancy. If there are doubts about the presence of metal parts in the body, the patient will have to inform the medical staff who will arrange radiograms to determine if the metal implants exist.
In the case of patients suffering from claustrophobia or particular situations, the examination can be carried out under sedation, subject to agreement with the Radiology Service at the moment. These situations should be reported at the time of booking.
What are the risks of Cardiac Nuclear Magnetic Resonance?
Cardiac MRI is not painful or dangerous. The only annoyance can be caused by the noise of the machinery in operation. Headphones will be provided to reduce perceived noise. There is a risk of a rare allergic reaction due to the contrast medium, which must be reported upon booking of the exam, if it is known.
How is Cardiac Magnetic Resonance Imaging performed?
The patient lies down on a bed, where electrodes for monitoring the heart beat will be applied. For the success of the magnetic resonance imaging, it is essential that the patient remains still and is able to hold their breath for about 10 seconds when asked to do so. The acquisitions are performed while holding the breath and with heart rate monitoring, in order to eliminate the artifacts from cardiac and respiratory movement. About halfway through the examination, a contrast agent is administered intravenously, if necessary. The duration of the exam varies from case to case, with an average of 30 minutes.

Hypertrophic cardiomyopathy with evidence of areas of late gadolinium enhancement at the junctions with the right ventricular free wall indicative of fibrotic replacement.
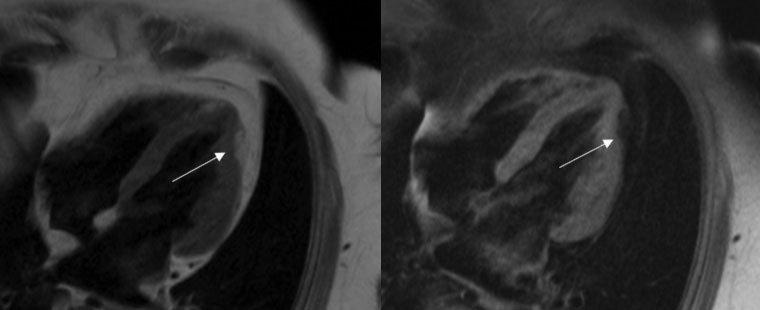
Biventricular arrhythmogenic dysplasia associated with an area of adipose infiltration in the distal lateral wall and apex of the left ventricle.
If you need to book a Cardiac Magnetic Resonance -> Information request and / or exam
Bibliography:
- Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. Bardy GH, Lee KL, Mark DB, Poole JE, Packer DL, Boineau R, Domanski M, Troutman C, Anderson J, Johnson G, McNulty SE, Clapp-Channing N, Davidson-Ray LD, Fraulo ES, Fishbein DP, Luceri RM, Ip JH; Sudden Cardiac Death in Heart Failure Trial (SCD-HeFT) Investigators. N Engl J Med. 2005 Jan 20;352(3):225-37.
- Long-term clinical course of patients after termination of ventricular tachyarrhythmia by an implanted defibrillator. Moss AJ, Greenberg H, Case RB, Zareba W, Hall WJ, Brown MW, Daubert JP, McNitt S, Andrews ML, Elkin AD; Multicenter Automatic Defibrillator Implantation Trial-II (MADIT-II) Research Group. Circulation. 2004 Dec 21;110(25):3760-5. Epub 2004 Dec 6.
- Scar extent evaluated by late gadolinium enhancement CMR: a powerful predictor of long term appropriate ICD therapy in patients with coronary artery disease. Alexandre J, Saloux E, Dugué AE, Lebon A, Lemaitre A, Roule V, Labombarda F, Provost N, Gomes S, Scanu P, Milliez P. J Cardiovasc Magn Reson. 2013 Jan 19;15:12. doi: 10.1186/1532-429X-15-12
- Assessment of myocardial deformation with cardiac magnetic resonance strain imaging improves risk stratification in patients with dilated cardiomyopathy. Buss SJ, Breuninger K, Lehrke S, Voss A, Galuschky C, Lossnitzer D, Andre F, Ehlermann P, Franke J, Taeger T, Frankenstein L, Steen H, Meder B, Giannitsis E, Katus HA, Korosoglou G. Eur Heart J Cardiovasc Imaging. 2015 Mar;16(3):307-15. doi: 10.1093/ehjci/jeu181. Epub 2014 Sep 21
- Prognostic Value of LGE-CMR in HCM: A Meta-Analysis. Weng Z, Yao J, Chan RH, He J, Yang X, Zhou Y, He Y. JACC Cardiovasc Imaging. 2016 Dec;9(12):1392-1402. doi: 10.1016/j.jcmg.2016.02.031. Epub 2016 Jul 20. Review.
- Role of cardiovascular magnetic resonance imaging in arrhythmogenic right ventricular dysplasia. Jain A, Tandri H, Calkins H, Bluemke DA.m J Cardiovasc Magn Reson. 2008 Jun 20;10:32. doi: 10.1186/1532-429X-10-32. Review
- Prognosis of Myocardial Damage in Sarcoidosis Patients With Preserved Left Ventricular Ejection Fraction: Risk Stratification Using Cardiovascular Magnetic Resonance. Murtagh G, Laffin LJ, Beshai JF, Maffessanti F, Bonham CA, Patel AV, Yu Z, Addetia K, Mor-Avi V, Moss JD, Hogarth DK, Sweiss NJ, Lang RM, Patel AR. Circ Cardiovasc Imaging. 2016 Jan;9(1):e003738. doi: 10.1161/CIRCIMAGING.115.003738.
- Cardiovascular magnetic resonance predictors of clinicaloutcome in patients with suspected acute myocarditis. Sanguineti F, Garot P, Mana M, O’h-Ici D, Hovasse T, Unterseeh T, Louvard Y, Troussier X, Morice MC, Garot J. J Cardiovasc Magn Reson. 2015 Aug 29;17:78. doi: 10.1186/s12968-015-0185-2.
- Prediction of cardiac complications for thalassemia major in the widespread cardiac magnetic resonance era: a prospective multicentre study by a multi-parametric approach. Pepe A, Meloni A, Rossi G, Midiri M, Missere M, Valeri G, Sorrentino F, D’Ascola DG, Spasiano A, Filosa A, Cuccia L, Dello Iacono N, Forni G, Caruso V, Maggio A, Pitrolo L, Peluso A, De Marchi D, Positano V, Wood JC. Eur Heart J Cardiovasc Imaging. 2018 Mar 1;19(3):299-309. doi: 10.1093/ehjci/jex012
- Cardiovascular magnetic resonance characterization of mitral valve prolapse. Han Y, Peters DC, Salton CJ, Bzymek D, Nezafat R, Goddu B, Kissinger KV, Zimetbaum PJ, Manning WJ, Yeon SB. JACC Cardiovasc Imaging. 2008 May;1(3):294-303. doi: 10.1016/j.jcmg.2008.01.013
- Ventricular size and function assessed by cardiac MRI predict major adverse clinical outcomes late after tetralogy of Fallot repair. Knauth AL, Gauvreau K, Powell AJ, Landzberg MJ, Walsh EP, Lock JE, del Nido PJ, Geva T. Heart. 2008 Feb;94(2):211-6. Epub 2006 Nov 29.
