Antiarrhythmic drugs
Antiarrhythmic Drugs are a group of pharmaceuticals that are used to suppress abnormal rhythms of the hear.
Indice dell'articolo
ANTIARRHYTHMIC DRUGS
The choice to start an antiarrhythmic treatment depends on the nature, severity of the arrhythmia, and the possible effect on any other cardiological problems. Generally, any underlying diseases, such as high blood pressure, heart failure, or thyroid disease, are treated first.
These drugs can be administered in acute situations, for example to stop an arrhythmia, such as paroxysmal supraventricular tachycardias, atrial fibrillation, or ventricular tachycardias (so-called “pharmacological cardioversion”). These drugs can also be used for chronic therapies, to control and reduce the incidence of arrhythmias (such as supraventricular or ventricular extrasystoles or atrial fibrillation).
Patients taking antiarrhythmic drugs must be followed meticulously to promptly identify the appearance of any side effects, and in particular the recurrence of any arrhythmias similar to those for which the antiarrhythmic drug has been prescribed, or the onset of new rhythm disorders that in some rare cases can be caused by antiarrhythmic drugs (so-called pro-arrhythmic effect).

HOW ARE ANTIARRHYTHMIC DRUGS CLASSIFIED?
Antiarrhythmic drugs are classified according to a special classification, called the Vaughan Williams Classification:
| Class I: inhibition of rapid sodium channels. |
|
| Ia subgroup (quinidine, disopyramide, procainamide) |
|
|
|
| Ib subgroup (lidocaine, mexiletine, diphenylhydantoin) |
|
|
|
| Ic subgroup (flecainide, propafenone, cibenzoline) |
|
|
|
| Class II: Blockers of beta adrenergic receptors |
|
|
|
|
| Class III: Blockers of the potassium channels iK (amiodarone, bretilio, sotalol) |
|
|
|
| Class IV: slow calcium channel inhibitors (verapamil) |
|
|
|
|
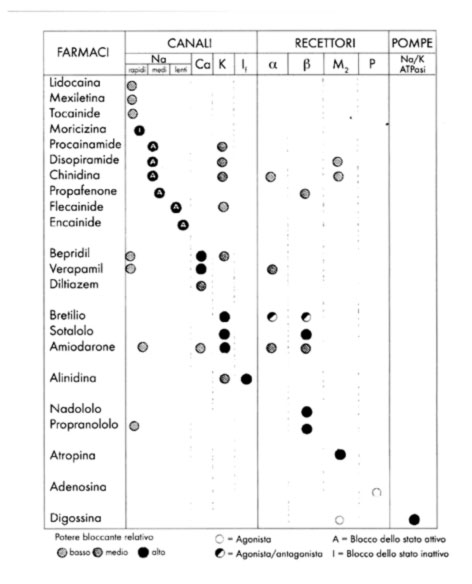
In addition to the Vaugham-Williams classification, there is also a classification called “Sicilian Gambit”, proposed by P.J. Schwartz in 2005, which proposes a synoptic view of the electrophysiological properties of antiarrhythmic drugs.
HOW DO ANTIARRHYTHMIC DRUGS WORK?
- Class Ia antiarrhythmic drugs (for example quinidine) block the K channels, repolarizing, and on the ECG this effect is evident as an extension of the QT interval, even for normal frequencies. Therefore, these drugs are contraindicated in long QT syndrome, and may instead be indicated in short QT syndrome and Brugada syndrome. Class Ia drugs are used to suppress atrial premature beats (APB), ventricular premature beats (VPB), supraventricular tachycardias, ventricular tachycardias, atrial fibrillation (FA), and atrial flutter.
- Class Ic antiarrhythmic drugs (e.g. Flecainide, Ajmaline and Propafenone) are more powerful antiarrhythmics than class Ia or Ib. Ic class drugs do not directly block the K channels and do not generally prolong the duration of the QT interval. Ic class drugs are used for the suppression of premature atrial and premature ventricular beats, supraventricular tachycardias, paroxysmal atrial fibrillation, atrial flutter and ventricular fibrillation. Class Ic drugs can depress ventricular function and are not recommended in case of myocardial dysfunction or ischemic heart disease.
Class II antiarrhythmic drugs are beta-blockers and mainly act on tissues with slow channels (sinus-atrial and atrioventricular node), where they reduce automation, conduction speed and increase the refractory period. Therefore, the heart rate drops, the PR interval lengthens, and the atrioventricular node conducts rapid atrial depolarizations at a lower rate. Class II drugs are used mainly to treat supraventricular tachycardias, including sinus tachycardia, re-entry tachycardias of the atrioventricular node, atrial fibrillation and atrial flutter. These drugs are also used to treat ventricular tachycardia, increase the ventricular fibrillation threshold in ischemic cells and reduce the ventricular pro-arrhythmic effects of beta-adrenergic receptor stimulation. Beta blocker drugs are also used for the treatment of heart failure, ischemic heart disease and high blood pressure. Beta blockers can also be used in the treatment of glaucoma, thyrotoxicosis, somatic manifestations of anxiety, essential tremor and in the prophylactic treatment of migraine. Beta blockers are generally well tolerated; adverse effects include apathy, sleep disturbances and gastrointestinal disturbances. Beta-blockers are divided into cardioselective beta 1 receptors (mainly located at the cardiac, renal and ocular levels), are non-cardioselective, and are endowed with intrinsic sympathomimetic activity. Non-cardioselective beta-blockers are contraindicated in patients with pneumopathies with bronchial hyperreactivity.
| Beta 1-selective beta blockers | Beta blockers not selective for beta 1 | Beta-blockers with sympathetic mimetic activity (ISA) |
| Acebutolol | Propanolol | Acebutolol |
| Atenolol (water soluble) | Nadolol | Pindolol |
| Betaxolol | Sotalol | Oxprenolol |
| Bisoprolol | Carvedilol | Celiprolol |
| Nebivolol | Alprenolol | |
| Metoprolol | Labetalol | |
| Cetamolol | Timolol | |
| Esmolol | ||
| Practolol |
- Class III drugs (amiodarone and sotalol) are membrane stabilizing drugs, mainly blocking the K channels, which prolong the duration of the action potential and the refractoriness in the tissues with both slow and fast channels. As the action potential is prolonged, automation is reduced. The predominant effect on the ECG is lengthening of the QT interval. These drugs are used to treat both supraventricular and ventricular tachycardias. Class III drugs can also be used in cases of myocardial dysfunction and ischemic heart disease. In particular, amiodarone can cause thyroid dysfunction (both hypo and hyperthyroidism). Therefore, thyroid hormones must be regularly monitored during amiodarone therapy.
- Class IV drugs are non-dihydropyridine Ca-antagonists (Verapamil), which depress the Ca-dependent action potentials in tissues with slow channels, and, therefore, reduce the automation, slow the conduction speed, and prolong the refractoriness. Heart rate decreases, the PR interval lengthens and the atrioventricular node leads to rapid atrial depolarizations at a lower rate. These drugs are mainly used to treat supraventricular tachycardias, or to slow rapid atrial fibrillation or atrial flutter.
It should be noted that digoxin and adenosine are not included in the Vaughan Williams classification.
- Digoxin shortens the atrial and ventricular refractory periods and is vagotonic, thus prolonging conduction along the atrioventricular node and its refractory period. Digoxin is currently used primarily in pediatric arrhythmias and chronic atrial fibrillation to improve rate control, particularly in patients with cardiac dysfunction.
- Adenosine slows down or blocks atrioventricular nodal conduction and is used only in an acute situation to stop tachyarrhythmias that depend on atrioventricular nodal conduction for their maintenance.
WHAT IS THE PROARITHMIC EFFECT?
Class Ia drugs, in predisposed patients, may cause prolongation of the QT interval and cause torsade de pointes type ventricular tachycardia. Class Ia drugs can organize and slow down atrial tachyarrhythmias in such a way as to allow 1:1 atrioventricular conduction with a marked increase in the ventricular response.
Class Ic drugs, in predisposed subjects, can induce the Brugada ECG pattern and favor the onset of ventricular tachyarrhythmias. Thus, it may happen that the diagnosis of Brugada syndrome occurs during therapy with Class Ic drugs, which may be administered, for example, for the prevention or cardioversion of atrial fibrillation. In predisposed patients, Class Ic drugs can cause prolongation of the QT interval and cause torsade de pointes type ventricular tachycardia. Finally, Class Ic drugs can organize and slow down atrial tachyarrhythmias in such a way as to allow 1:1 atrioventricular conduction with a marked increase in the ventricular response.
Class III drugs, which prolong the QT interval, have a risk of ventricular proarrhythmia, especially torsade de pointes type ventricular tachycardia, and are not used in patients with this type of tachycardia.
HOW IS THE MONITORING OF ANTI-ARRHYTHMIC DRUGS PERFORMED?
Patients taking antiarrhythmic drugs should be carefully monitored to identify any recurrence or worsening of the arrhythmic picture. For example, patients taking antiarrhythmic drugs should be educated to check their pulse to promptly identify any pathological rhythms.
Patients must undergo electrocardiographic checks using the various ECG recording methods available, to be evaluated according to the clinical picture: basal ECG, dynamic ECG according to Holter, prolonged multi-week Holter ECG, Cardiotelephone.
In case of patients with implantable cardiac devices (implantable loop recorder, pacemaker, cardiac defibrillator, resynchronizers) the patient can be followed by remote monitoring of cardiac devices.
