Implantable Cardioverter Defibrillator (ICD)
Indice dell'articolo
WHAT IS THE IMPLANTABLE CARDIAC DEFIBRILLATOR?
The implantable cardiac defibrillator (ICD) is a device used to recognize and treat ventricular arrhythmias, specifically ventricular tachycardia and ventricular fibrillation, which would be potentially fatal if not interrupted promptly. The anti-tachycardia function of the ICD consists of delivering pulses or shocks to stop ventricular arrhythmias, and thus preventing syncopal episodes and sudden cardiac death. In addition to the anti-tachycardia function, the ICD is equipped with anti-bradycardia functions, so they are able to stimulate the heart if the heart rate becomes too low (similar to the pacemaker).
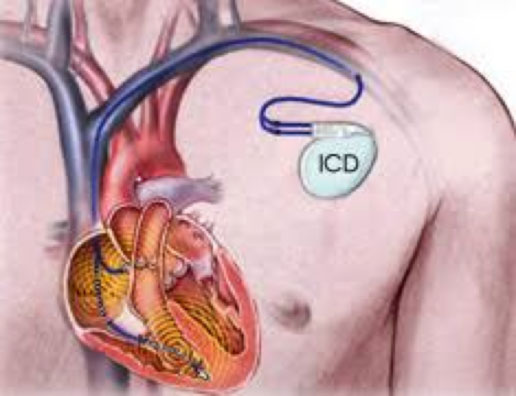
The first ICD was developed in the 70’s, mainly by Marcel Mirowski, of Baltimore. The first implants were performed in the abdominal area, and the electrodes for defibrillation were applied to the surface of the heart (epicardium). Currently, the ICD is surgically implanted subcutaneously in the pectoral region, preferably on the left, positioning the electrodes intravenously in the right ventricle, and possibly also in the right atrium (in bicameral ICDs), and in the veins at the left ventricle surface (in the case of ICD resynchronizers, ICD-CRT). Currently, in addition to the classic intravenous ICDs, there are also subcutaneous ICDs, which have specific clinical indications.

FOR WHICH PATIENTS IS THE ICD RECOMMENDED?
Patients who are candidates for an ICD implant can be divided into two categories:
- SECONDARY prevention patients, i.e. patients who have already had ventricular cardiac arrhythmias:
- patients who survived a first cardiac arrest due to ventricular fibrillation
- patients with very rapid sustained ventricular tachycardias that cause loss of consciousness, not controlled by medical therapy and / or other electrical therapies, such as catheter ablation.
- Patients in PRIMARY prevention, i.e. patients who have not already had malignant ventricular arrhythmias, but are considered at high risk of developing such arrhythmias:
- patients with ischemic heart disease, with low ejection fraction (FE <35%) and presence of heart failure
- patients presenting with rare clinical conditions, which according to precise individual risk stratification criteria are considered to be at high risk of sudden cardiac death according to current guidelines, such as long QT syndrome, Brugada syndrome, arrhythmogenic dysplasia of the right ventricle, hypertrophic cardiomyopathy, dilated cardiomyopathy, non-compact myocardium
HOW DOES THE IMPLANTATION OF AN INTRAVENOUS ICD BEGIN?
Similarly to pacemaker implantation, ICD implantation is almost always performed under local anesthesia and lasts about 60 minutes on average. The procedure is generally well tolerated; in case of pain the dosage of local anesthetic is increased or, in rare cases, for example in pediatric patients, deep sedation is performed with anesthetic assistance.
The first phase consists of the positioning of the leads, that is the “electric wires” that stimulate the heart; their number can vary from one to three depending on the type of device that needs to be implanted. The leads are inserted through the cephalic vein and / or the subclavian vein (usually left, depending on the anatomy of the individual patient) and are pushed to the heart under the fluoroscopic guide (x-rays).
The main catheter (defibrillation catheter) is placed at the tip of the right ventricle (single-chamber ICD, or ICD-VR). In some cases, a second catheter is also implanted in the right atrium (ICD Bicameral, ICD-DR). In cases where cardiac resynchronization is required, a third cataract can be implanted through the coronary sinus in the cardiac veins to stimulate the left ventricle wall (ICD-CRT or CRT-D). The electrodes are positioned, with the help of dedicated software programs, at the points where they sense the cardiac activity and where they are able to stimulate the heart using the lowest possible energy.
After checking the stability and effectiveness of the stimulation, the catheter (or catheters) are fixed and connected to the stimulator case. By a small incision, the defibrillator is inserted into the pectoral region subcutaneously or under the pectoral muscle.
At this point, it is necessary to test the correct functioning of the system. During this test, the cardiologist causes the onset of a rapid ventricular arrhythmia and causes the defibrillator to recognize and treat it appropriately and effectively. In this phase, a deep sedation is used to avoid the patient from feeling unpleasant sensations related to the onset of the arrhythmia and the consequent electric therapy.
The incision is subsequently closed with suture thread (often resorbable, so without the need for subsequent removal of the stitches). A chest X-ray is also performed in order to evaluate the positioning of the leads. After the implant, after a brief period of lodging, the electronic control of the device is performed, and then the patient is discharged the day after the implant.
WHAT ARE THE COMPLICATIONS RELATED TO THE ICD IMPLANT?
Complications related to ICD implantation are rare and generally not serious. The most frequent is the formation of a local hematoma during implantation (which is generally reabsorbed spontaneously within a few days).
In very rare cases, it is possible that damage is caused to the venous vessels used for access (with consequent thrombosis and possible phlebitis), an eventual pneumothorax in the case of puncture of the subclavian vein (passage of air inside the pleural cavity, in most cases asymptomatic and self-solvent, rarely requiring temporary drainage positioning), a possible pericardial effusion secondary to perforation of the myocardial wall of the electrocatheters (very rare occurrence, which in some cases may require temporary drainage positioning).
A possible complication, which generally occurs in complex cases with multiple pathologies and multiple device replacements, is the infection of the device pocket or the endocarditis starting from the leads. These infections are very difficult to treat and may require the removal of the entire ICD.
HOW DO THE CHECKS GO AFTER THE ICD IMPLANTATION?
About 7-10 days after the implantation, an out-patient surgical wound assessment is performed and, in the case of non-absorbable suture thread, the stitches are removed.
Patients with implantable defibrillators must subsequently undergo a regular (generally every six months) check of the device, according to the recommended timing based on the specific pathology.
It is currently recommended by the current guidelines that ICDs be checked regularly through remote telemetry control or remote monitoring of cardiac devices.
| Even if this method is not yet reimbursed by the NHS, in our center almost all implanted patients are followed free of charge through Remote Monitoring. Therefore, all patients at the time of discharge are given or sent with the dedicated modem for Remote Monitoring. |
If you want to know more > Remote monitoring of devices
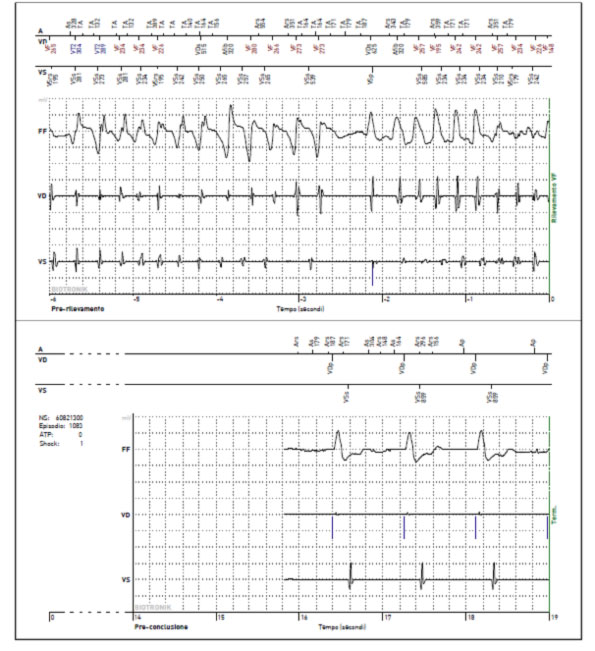
WHAT HAPPENS WHEN AN ICD DETECTS AN ARRHYTHMIA?
The ICD is programmed to recognize certain ventricular cardiac arrhythmias and intervene when necessary to stop the arrhythmia and restore the normal rhythm. The intervention of the ICD can take place in the following ways:
- Anti-tachycardia pacing (ATP): in the event that the arrhythmia is fast and regular (ventricular tachycardia) the ICD attempts to deliver rapid pulse trains to stop the arrhythmia. Such therapies are generally felt by the patient, or are felt as mild palpitations
- Cardioversion (CV): in the case of ventricular tachycardias that are not interrupted by the ATP, the ICD can deliver a low or medium energy shock (usually 4-10 Joules), which is generally not felt or felt like a thud in the chest
- Defibrillation (DC): in the event that the arrhythmia is very fast and chaotic, typically in ventricular fibrillation (VF), the ICD delivers a high-energy discharge (generally 30-40 Joules), which is felt, if the patient is still conscious, like a big blow or a kick in the chest. If the VF is not interrupted at the first shock, the ICD can deliver up to 6 consecutive shocks.
Anti-bradycardia pacing: if the heart rate is too slow, the ICD can deliver a stimulation to the atrium or ventricle, behaving like a pacemaker.
WHAT YOU NEED TO DO AFTER A SHOCK
| After an effective defibrillation, the patient may feel well, but it is still useful to contact the center to carry out a check on how the ICD intervened for the arrhythmic event. |
This check can be performed in the hospital or directly from home through Remote Monitoring. This check also serves to verify whether it is necessary to carry out further diagnostic tests (for example coronary angiography) or to modify the drug therapy or to schedule the ablation of the arrhythmia.
In the event that the ICD mistakenly interprets the presence of a ventricular arrhythmia (which can occur in the case of high-frequency rhythms, due to sinus tachycardia or supraventricular arrhythmias including atrial fibrillation, or due to the recognition of anomalous signals due to rupture of an electrocatheter or an electrical interference) an inappropriate shock can occur. In this case, it is always necessary to investigate the device, either directly in the hospital or remotely.
DOES THE ICD IMPLANT LIMIT NORMAL DAILY ACTIVITIES?
Patients undergoing an ICD implant usually return to normal daily activities within a very short time after the procedure. Within the first three months after implantation, it is generally advised to avoid intense physical activity, including carrying heavy loads. Later, the patient can gradually return to his or her normal lifestyle and resume the physical activity he or she was used to after completing his or her recovery period.
Sexual activity can also be resumed normally after ICD implantation. Sexual activity leads to an increase in heart rate, which in very rare cases can lead to an erroneous recognition of the arrhythmia by the device, which can lead, in extreme cases, to the delivery of inappropriate therapies (including inappropriate shocks). If this happens, the ICD must be reprogrammed, and in any case the shock is not a danger to the partner.
Car driving can be resumed with some limitations (see ICD and driving license). The use of seat belts in cars is not recommended for patients with ICDs (such as in patients with pacemakers).
IT IS POSSIBLE TO ENGAGE IN PHYSICAL AND SPORTS ACTIVITY AFTER ICD IMPLANTATION?
After the first three months, in general, the patient can return to non-competitive physical activity. In general, caution should be exercised in sports, such as tennis, golf, or swimming in the first few months after implantation, particularly involving the upper limbs, avoiding excessive extension that can cause dislocations of the leads.
In general, physical activity leads to an increase in heart rate, which in rare cases can lead to an erroneous recognition of the arrhythmia by the device, which can lead in extreme cases to the delivery of inappropriate therapies (including inappropriate shocks). To avoid this risk, personalized relatively delayed recognition is planned for young and athletic people.
Then there are some sports that have a high “intrinsic risk”, in which the loss of control due to an arrhythmia and shock, even for a few seconds, can have potentially serious effects, such as motoring, mountaineering, underwater sports, parachuting, etc.
Particular caution must be exercised in sports that involve violent physical contact (for example, football, rugby, wrestling), or a risk of falling (for example, downhill skiing) or collisions at the site of implantation (boxing, judo) as this could damage the device or the leads.
IT IS POSSIBLE TO TRAVEL AFTER ICD IMPLANTATION?
Most patients undergoing cardiac device implantation can travel without limitations, unless there are contraindications related to the underlying clinical condition.
Before leaving, it is advisable to consult your doctor in reference to:
- Specific health or behavioral recommendations
- How to behave in the event of discomfort or appearance of symptoms
- How to find a cardiology institute, emergency service, or medical assistance in your destination
IT IS POSSIBLE TO GO THROUGH SECURITY SCREENINGS (AIRPORTS, BANKS, ETC) AFTER ICD IMPLANTATION?
Before crossing a security checkpoint, especially at the airport, the patient must inform the security staff that he / she has a cardiac device and present the identification certificate. Then the patient will go through the security machine at a normal pace, taking care to leave the machine if he or she feels dizzy or has an accelerated heartbeat.
The airport security systems are magnetic detectors, and therefore they will launch an alarm signal when they detect the metal casing of the cardiac device. If the surveillance staff uses a hand-held metal detector to check the passenger, ask the operator not to place or pass the instrument over the cardiac device.
ARE ELECTROMAGNETIC FIELDS DANGEROUS FOR ICD PATIENTS?
Some electrically powered appliances with magnets can create energy fields, which can alter the normal operation of the ICD.
The greater the proximity of the object, and the greater the energy of the device, the greater will be the electromagnetic field that can be formed. In most cases, electromagnetic energy fields are limited and weak and do not affect the functioning of the cardiac device, but electrical equipment with a stronger energy field, such as welding machines, chainsaws, mowers, and other industrial machinery, can produce interference and alter the normal functioning of the ICD.
Devices that emit low-energy electromagnetic waves (such as microwave ovens, mobile phones, or computers) can be used safely, but it is useful to maintain a certain distance between these devices and the ICD (at least 30 cm), so, for example, it’s better to avoid putting your smartphone in your jacket pocket or getting too close to the microwave oven.
| It is important to check the foundation system of your home or of houses that are rented (for example for holidays), to check that there are no energy leaks that can produce electrical interference and alter the normal operation of the ICD. |
WHICH MEDICAL AND ORTHODONTIC PROCEDURES MUST BE AVOIDED AFTER ICD IMPLANTATION?
Before undergoing any medical procedure, always inform the doctor, dentist or technician of the presence of the ICD. Before performing the procedure, these professionals may need to contact the cardiologist, particularly if the procedure is new or unusual.
Some procedures may affect the functioning of the cardiac device and therefore require precautionary measures to avoid or minimize any effects on the patient or on the device itself.
PROHIBITED MEDICAL PROCEDURES
Individuals with ICDs should not be subjected to the following medical procedures, unless the ICD is properly programmed or temporarily deactivated:
- Trans-catheter radiofrequency ablation
- Diathermic treatment (with shortwave high frequency, or microwave)
- MRI exams (magnetic resonance imaging) or MRA (angiography with magnetic resonance)
MEDICAL PROCEDURES TO BE CARRIED OUT WITH PRECAUTION
Some medical procedures can be performed safely with the adoption of specific precautions by the doctor to avoid potential problems with device operation or interference:
- Computerized axial tomography (TC o TAC)
- Diagnostic ultrasound
- Electrocautery
- Electrolysis
- External defibrillation and elective cardioversion
- High energy radiotherapy
- Hyperbaric oxygen therapy (HBOT)
- Lithotripsy
- Ultrasound therapy
- Transcutaneous electrical nerve stimulation (TENS)
- Transmission circuits for hearing aids
ALLOWED MEDICAL PROCEDURES
There are many medical procedures that do not affect the functioning of the ICD:
- orthodontic procedures involving the use of drills or ultrasound probes for oral hygiene and oral cavity radiographs.
- diagnostic radiographs, for example for chest X-rays and mammograms.
However, the tools used for these procedures must be used correctly and properly stored. However, it is advisable to consult your doctor to assess the potential risks and benefits of the medical procedure.
WHAT ARE THE LIMITATIONS ON DRIVING AFTER ICD IMPLANTATION?
The current European guidelines prohibit commercial vehicle driving (in practice for driving licenses C, D, E). Conversely, regarding driving private cars (driving license B), the guidelines prohibit driving for 6 months after implantation of an ICD and, if there were no interventions or syncopal arrhythmias during the 6 months, the patient can drive. In case of ICD intervention, the observation period continues for a further 6 months. This interval is considered sufficient to assess the frequency and characteristics of the events. Abstention from driving becomes permanent in the case of frequent interventions of the ICD.

The presence of an ICD testifies in and of itself that a risk of transient loss of consciousness exists. It follows that each Commission has a certain discretion in giving or not giving the permission for driving to each patient on an individual basis, based on the specific individual risk of loss of consciousness, given that there could be a liability for the Commission itself in the event of an accident caused by a loss of consciousness in ICD carriers.
Reference:
- Jung W, Anderson M, Camm AJ, et al. Recommendations for driving of patients with implantable cardioverter defibrillators. Study Group on ‘ICD and Driving’ of the Working Groups on Cardiac Pacing and Arrhythmias of the European Society of Cardiology. Eur Heart J 1997;18(8):1210-1219.
- Roberto Mantovan, Antonio Raviele, Pietro Delise, Paolo Stritoni. Patente di guida e defibrillatore impiantabile: dalla parte del cardiologo, del giurista… o del paziente? G Ital Aritmol Cardiostim 2002;2:85-88
WHAT HAPPENS IN CASE OF EXHAUSTMENT OR MALFUNCTION OF THE ICD?
In the event that during the checks (carried out in the clinic or remotely) the exhaustion of the battery of the device is ascertained, replacement is scheduled, which is carried out after a brief hospitalization (sometimes in day hospital). In general, the replacement takes place through the incision of the skin, with the removal of the old device and the repositioning of a new device in the same pocket, after reconnecting the leads, which are not generally replaced.
On the other hand, if a malfunction or failure of a lead is detected, a check of the implant may be necessary, with the replacement and repositioning of the leads. This check is carried out after hospitalization, and the specific procedures required will be explained directly by the doctors on a case-by-case basis.
